Abstract
Background
Measurable residual disease (MRD) is associated with inferior outcomes in patients with acute myeloid leukemia (AML). MRD monitoring enhances risk stratification and may guide therapeutic intervention. Post-induction MRD is frequently cleared with further therapy and the clearance may lead to better outcomes. In contrast, persistent MRD is associated with poor outcomes. At present it is not possible to predict which patients are likely to clear MRD with further therapy. Here we report a simple, objective, widely applicable and quantitative MFC approach using the ratio of blast/PDC to predict persistent MRD and poor outcomes in AML.
Patients and Methods
A cohort of 136 adult patients with a confirmed diagnosis of AML by WHO criteria who underwent standard induction therapy at a single center between 4/2014 and 9/2017 was initially included. 69 patients achieved complete morphologic remission (36 MRD-neg. and 33 MRD-pos.). MRD status was assessed by MFC using a different from normal (DfN) approach. PDC were quantified as the percent of total WBC by flow cytometry based on low side scatter, moderate CD45, CD303, bright CD123 and HLA-DR expression.
Results
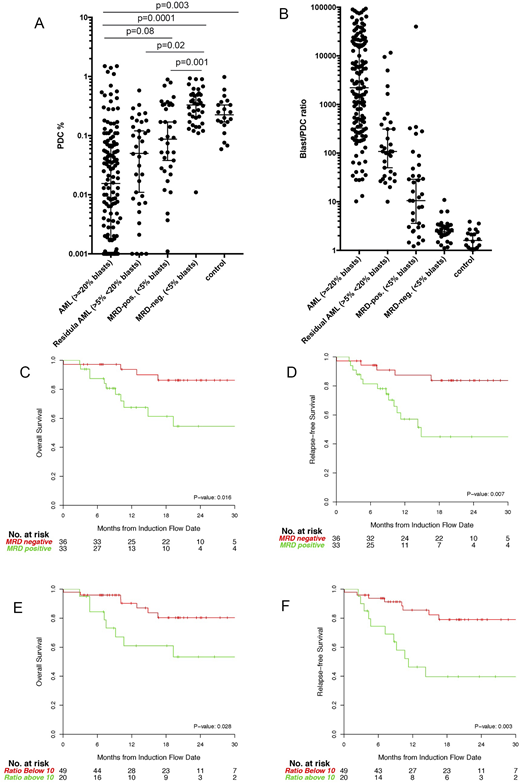
The proportion of PDC was markedly decreased in patients with AML (≥20% blasts) (N=136) with a median of 0.016% (interquartile range IQR: 0.0019%-0.071%, Figure 1A), more than 10-fold lower than observed in normal controls (median 0.23%, IQR 0.17%-0.34%) (N=20). While there was no difference between MRD-neg. and normal control groups (median 0.31%, IQR: 0.17%-0.49%; vs. 0.28%, IQR: 0.17%-0.34%), MRD-pos. group had significantly reduced PDC proportion compared to the control (median 0.074%, IQR: 0.022%-0.33%, Wilcoxon rank sum, p=0.019). In an attempt to achieve better separation and to eliminate possible effects of hemodilution, the ratio of blast/PDC was calculated by using the proportions of blasts and PDCs out of total WBCs as quantitated by flow cytometry. A cut-off threshold of the blast/PDC ratio of 10 was chosen to separate each group (Figure 1B). Importantly, a ratio cut-off of 10 had a corresponding specificity of 97.4% for predicting MRD positivity status.
MRD positivity was significantly associated with inferior overall survival (OS) and relapse-free survival (RFS) in our study cohort (OS HR 4.11 (95% CI: 1.30-13.03), p=0.016; RFS HR 4.20 (95% CI: 1.49-11.82), p=0.007, Figure 1C and D). The 2-year cumulative incidence of relapse in the MRD-neg. group compared to MRD-pos. group was 10% (95% CI: 2-24%) vs. 37% (95% CI: 18-56%, p=0.014). Importantly, blast/PDC ratio ≥10 was also strongly associated with inferior OS and RFS (OS HR 3.12 (95% CI: 1.13-8.60), p= 0.028; RFS HR 4.05 (95% CI: 1.63-10.11), p=0.003, Figure 1E and F), which is similar in magnitude to MRD positivity. Furthermore, MRD-pos. patients with blast/PDC ratio <10 had 4 times higher MRD clearance rate than MRD-pos. patients with a ratio ≥10 (6/11, 55% vs 2/17, 12%, Fisher exactp=0.02).
Conclusion
We have established an objective and quantitative MFC method to risk stratify post induction AML patients by risk for relapse, MRD clearance and likelihood of survival. Loss of PDC correlates with residual leukemia, is highly specific for MRD positivity in post-induction patients, and strongly predicts poorer overall survival and higher likelihood of relapse. Loss of PDC also predicts persistent MRD in post-induction MRD-pos. patients despite further therapy, suggesting that MRD-pos. patients with normal PDC may benefit from further therapy prior to transplant, while MRD-pos. patients with loss of PDC may not.
Goldberg:AROG: Research Funding; Pfizer: Research Funding; Celgene: Consultancy. Geyer:Dava Oncology: Honoraria. Levine:Isoplexis: Equity Ownership; C4 Therapeutics: Equity Ownership; Gilead: Honoraria; Qiagen: Equity Ownership, Membership on an entity's Board of Directors or advisory committees; Prelude: Research Funding; Imago: Equity Ownership; Roche: Consultancy, Research Funding; Loxo: Consultancy, Equity Ownership; Celgene: Consultancy, Research Funding; Novartis: Consultancy; Epizyme: Patents & Royalties; Janssen: Consultancy, Honoraria. Tallman:BioSight: Other: Advisory board; AROG: Research Funding; AbbVie: Research Funding; Cellerant: Research Funding; ADC Therapeutics: Research Funding; Orsenix: Other: Advisory board; Daiichi-Sankyo: Other: Advisory board.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal